Patients should be able to see first contact physiotherapists (FCP) as easily as they can see GPs, but careful evaluation is essential to ensure it works well.
This was the message from Sarah Withers, CSP’s head of FCP implementation, during a presentation at the NHSE Mobilisation Conference, held in London on 25 September.
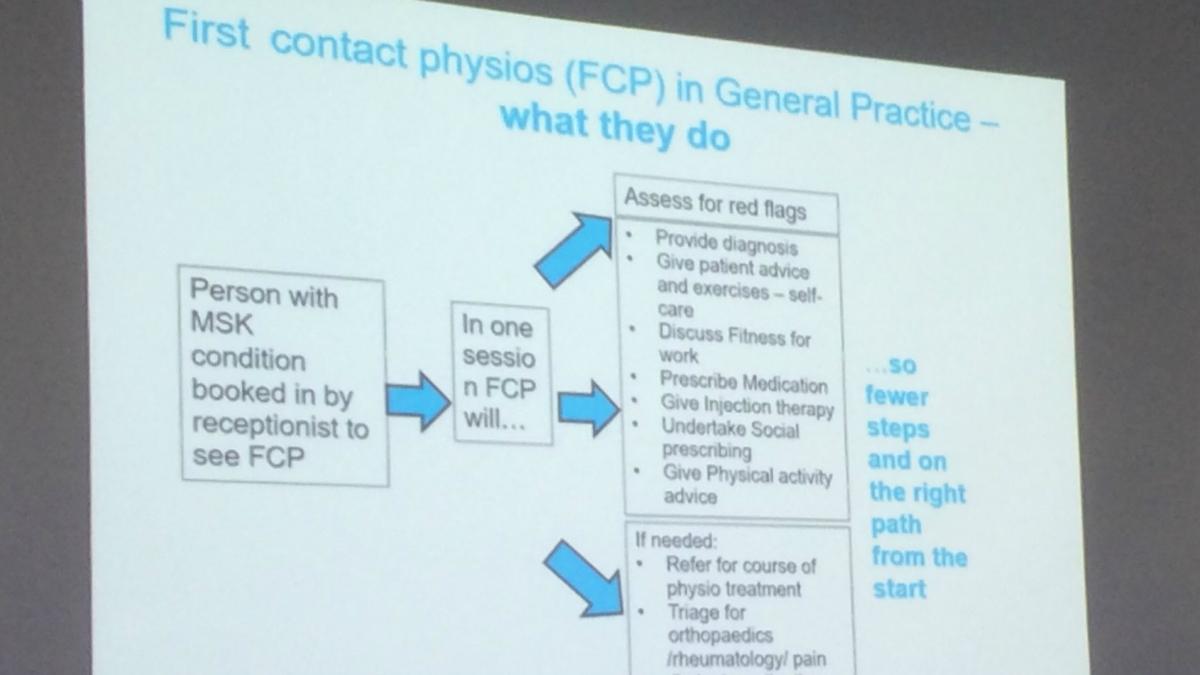
During the session, she outlined the essential steps required for successful FCP implementation, and highlighted how physiotherapists working as the first point of contact could benefit patients.
‘First contact physiotherapy can have a really positive impact on musculoskeletal care,’ she said.
‘It incorporates many approaches that we know are beneficial. These include the use of shared decision-making and personalised care, promoting self-management, incorporating biopsychosocial approaches and – crucially - using evidence based pathways right at the time when people first seek support.’
But to maximise its benefits Ms Withers emphasised that commissioners and service leads needed to consider all the factors that could influence the implementation of a FCP service.
‘Over the last few years, certain areas of the UK have developed FCP services in response to local population needs and we’ve seen that there is more than a single model of providing FCP services.
‘Now, through a three-phase evaluation plan, we have the opportunity to evaluate in a systematic manner the impact of FCP services on the flow of patients through primary and secondary care, the use of resources and the outcomes and experiences of patients, the primary care team and FCPs.’
Local context, knowledge and operational processes
Delegates heard there were three key areas for implementation, which will support effective evaluation of FCP.
‘These are the local context, which is broadly about relationships, expectations and understanding,’ said Ms Withers.
‘Knowledge, which is about what is required to integrate FCPs and services into existing primary and secondary care pathways
‘And operational processes, which depend on the primary care team approach, are fundamental to patient safety and capacity - these can feel like basic details although they have a significant impact.’
Ensuring effective FCP delivery
Not considering all three aspects could make it impossible to deliver an effective FCP service, Ms Withers warned, each of these areas overlaps and affects the ability of the FCP to deliver safe, person centred care.
‘For example if the practice team are not fully aware of the scope and breadth of an FCP service and role, problems may start at the front door, with fewer patients or a narrower group of patients being booked with the FCP, clearly reducing the impact on the GP workload before any intervention has begun,’ she explained.
‘If knowledge is lacking, in terms of accessing the normal referral pathways that the practice uses or could use, then the use of social interventions which promote self -management will be reduced.
‘And if operational processes are not ironed out, a lack of a chaperone or a protocol for the management of urgent results or referrals could impinge on patient safety.’
Email fcp@csp.org.uk to join CSP’s FCP network for the latest resources, support and networking opportunities.
Number of subscribers: 4



































