Physiotherapists can play a central role in ensuring patients with spondyloarthritis receive an early diagnosis and are treated appropriately, says consultant physiotherapist Carol McCrum.
Spondyloarthritis encompasses a group of inflammatory conditions with some shared clinical features. These conditions are important to recognise to enable early management to reduce the impacts and improve outcomes. A second article will appear in the future.
These conditions can have diverse symptoms and be difficult to identify. The average time to diagnosis spondyloarthritis is eight and a half years, despite a better understanding of these conditions, advances in imaging and effective treatments. These conditions are often mistaken as chronic back pain, tendonitis or joint problems. Symptoms can also be intermittent. They can move around peripheral areas and flare and settle, mimicking acute or recurrent back pain or tendon/joint problems.
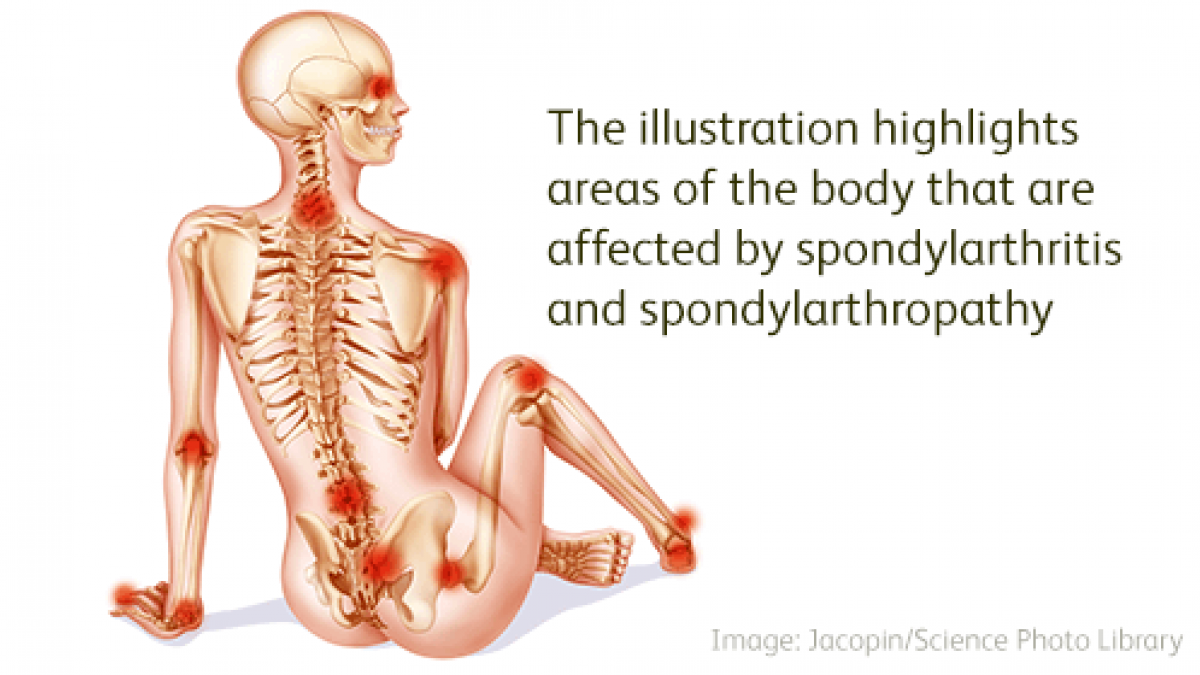
Spondyloarthritis can present with predominantly peripheral problems, including dactylitis (inflammation of a whole digit joints, tendons and entheses - 'sausage finger or toe'), enthesitis (inflammation at the tendon attachment to a bone), and joint pain/swelling, or predominantly axial problems (sacro-iliac joint/spine), or involving both regions.
Spondyloarthritis is often associated with extra-articular inflammatory conditions. These include skin/nail psoriasis, inflammatory bowel disease (Crohn's disease/ulcerative colitis) and uveitis (acute severe eye pain, eye redness, sensitivity to light or blurred vision). Some people may have several of these conditions or none (undifferentiated spondyloarthritis). These conditions may not be active, or only manifest later. Separate recommendations are offered for recognising axial and peripheral presentations, which relates to evidence for different signs and symptoms, risk factors, investigation strategies and treatment. However, both regions may be involved.
Spondyloarthritis conditions include:
- axial spondyloarthritis and ankylosing spondylitis
- psoriatic arthritis
- enteropathic arthritis, which is related to inflammatory bowel disease
- reactive arthritis, which is triggered by a recent gastrointestinal or genitourinary infection
- undifferentiated spondyloarthritis has no identified associations)
Recognition and referral of suspected axial spondyloarthritis
Refer patients to rheumatology if they have low back pain that started before the age of 45 years and has lasted longer than three months, and if four or more of the following points apply:
- low back pain started before the age of 35 years (increases likelihood of axial spondyloarthritis)
- waking during second half of the night because of symptoms
- buttock pain
- improvement with movement
- improvement with taking non-steroidal anti-inflammatory drugs (often within 48 hours)
- current or past enthesitis
- current or past psoriasis
- current or past arthritis
- first-degree relative with spondyloarthritis or psoriasis
If only three additional criteria are met, then HLA-B27 testing is recommended and referral to rheumatology if the result is positive. When screening criteria are not met but clinical suspicion remains, advise the person to seek re-assessment if new signs, symptoms or risk factors develop. This may be particularly appropriate if the person has or had psoriasis, inflammatory bowel disease or uveitis. While morning stiffness lacked sensitivity and specificity as a referral criterion for axial spondyloarthritis, prolonged morning stiffness (lasting more than 30 minutes) can be an important factor when an inflammatory disease is suspected.
Spondyloarthritis: key points
- it is often missed in non-specialist settings and mistaken as chronic back pain, tendonitis or joint problems
- assess for axial spondyloarthritis for back pain onset before 45 years and lasting more than three months
- ask about extra-articular conditions - psoriasis, inflammatory bowel disease, uveitis and a family history of psoriasis or spondyloarthritis
- axial spondyloarthritis affects women and men equally and people can be human leukocyte antigen negative
- MRI imaging should perform an inflammatory back pain protocol which includes sacro-iliac joints and spine
- be suspicious of peripheral spondyloarthritis if dactylitis, or persistent or multiple site enthesitis occurs, particularly with associated extra-articular risk factors
- inflammatory markers C-reactive protein and erythrocyte sedimentation rates may be normal
Peripheral spondyloarthritis
Peripheral spondyloarthritis is often misdiagnosed as an unrelated tendon or joint problem. Symptoms can often move around between areas or flare and settle. A person presenting with dactylitis should be referred to rheumatology.
Suspect peripheral spondyloarthritis in people who have enthesitis without apparent mechanical cause, and if the symptoms are persistent and occur in multiple sites. Other key factors include: back pain without apparent mechanical cause; current or past uveitis (acute anterior uveitis symptoms require immediate referral for same day ophthalmological assessment); current or past psoriasis; inflammatory bowel disease (Crohn's disease or ulcerative colitis); a first-degree relative with spondyloarthritis or psoriasis; gastrointestinal or genitourinary infection. For suspected undiagnosed psoriasis, follow the NICE guideline on psoriasis.
Blood tests
It is important not to rule out a diagnosis of spondyloarthritis on the basis of a negative human leukocyte antigen-B27 test. Inflammatory markers C-reactive protein and erythrocyte sedimentation rates can be normal.
Diagnostic imaging
The diagnosis of spondyloarthritis will be based on an evaluation of clinical features, blood tests and imaging findings. Imaging may involve X-ray, MRI or ultrasound depending on presentation, regions involved and other factors influencing imaging decisions.
Importantly, the MRI protocol to investigate for inflammatory back pain/sacroiliitis differs from standard lumbar spine MRI protocols.
The MRI protocol should perform T1 and short T1 inversion recovery (STIR) of both the sacroiliac joints (coronal oblique view) and cervical, thoracic and lumbar spine. If a disparity occurs between clinical suspicion and imaging findings, consider having the imaging reviewed by a specialist MSK radiologist. FL
Dr Carol McCrumis a consultant physiotherapist, East Sussex Healthcare NHS Trust, and a NICE fellow.
For more information: NICE guideline on Spondyloarthritis for 16s and over (2017) www.nice.org.uk/guidance/ng65
Author
Carol McCrum consultant physiotherapistNumber of subscribers: 2




































