The average national completion rates for pulmonary rehabilitation (PR) is 62 per cent and there is a national challenge to drive numbers up
In the face of the Covid-19 pandemic, the Greenwich pulmonary (PR) service used Quality Improvement (QI) methods to rapidly move their service online. With a mounting waiting list and an expectation that they would not be able to return to business as usual soon, they had to adapt. They selected a QI method to support their redesign with bold targets identified: to increase completion rates for the Greenwich PR programme participants to 50 per cent by December 2021, 60 per cent by December 2022 and 70 per cent by December 2023, aided by virtual PR as an alternative to the traditional supervised programme.
Helen Jefford, specialist physiotherapist in respiratory care, explains: ‘Our primary objective was to design a programme that was effective, safe and enjoyable.
‘But we also had a secondary objective to increase completion rates over a three-year period. The completion rate for the Greenwich PR programme was low at 40 per cent. We wanted to offer increased choice on how to access PR.’
The team called about 120 people waiting for PR to assess the appetite for a virtual offer, and as a result updated their processes to support an online package. In establishing the new offer, the team engaged in peer learning with cardiac rehabilitation colleagues about risk assessments, staff training and pathway redesign.
The team was mindful of the potential inequality and barrier to access for people without smart phones/tablets or computers so acquired two tablets which can be loaned to participants for the eight-week programme. This also enabled those participants to use the myCOPD app to support self-management.
Preliminary results of the virtual PR programme showed that 51 people enrolled - 26 of these completed the programme, with six people partially completing, 10 didn’t start the programme, and at the time of collecting this data nine people were actively engaged in the programme.
Overall, the completion rate for the virtual programme was 61 per cent and no adverse events have been reported.
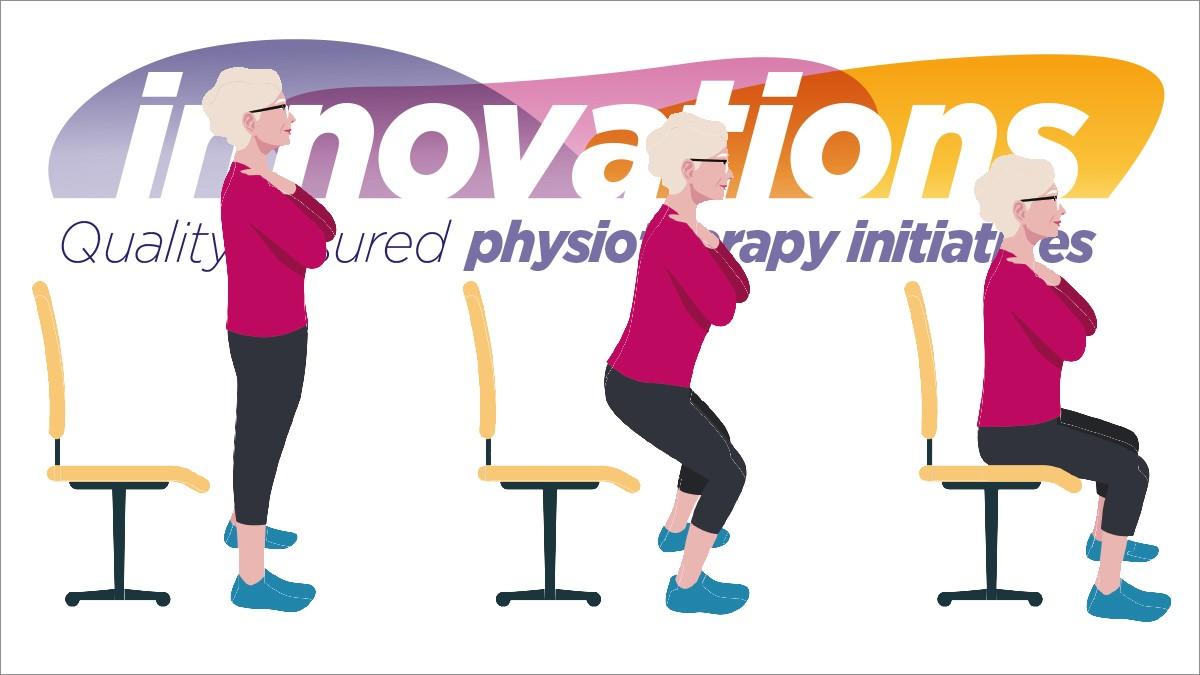
The current outcome data suggests that the new virtual model is a success and outcomes are comparable to in-person programme results, with a mean improvement of 5.75 in the one minute sit to stand test. And 61 per cent of people showed a reduction in their anxiety scores (GAD 7) and depression scores (PHQ-9).
As well as the positive outcomes, experience measures were also positive.
The team received encouraging feedback:
- ‘I feel less anxious to leave the house.’
- ‘It’s easier to have my family/carer join me when exercising.’
- ‘It’s easier to carry on with home exercise.’
While there was some initial cost outlay for a laptop, two tablets and 60 pulse oximeters, there were significant savings. Most notably, travel, parking and room hire costs.
With the QI method signalling the start of a continuous improvement process, further changes were explored in subsequent PDSA (plan, do, study, act) cycles.
Changes made so far, as part of the QI project to improve completion rates for example, are the introduction of text reminders to attend sessions or the increased 1:1 time spent supporting people in practising how to use the technology.
In conclusion, the team reported that with a menu-based option of care, they could confidently offer greater choice for the provision of pulmonary rehab as a therapeutic MDT intervention for people with a chronic lung condition.
Outcomes
- Overall the completion rate for the virtual programme was 61 per cent.
- 61 per cent of people showed a reduction in their anxiety scores (GAD 7) and depression scores (PHQ-9).
- There was a mean improvement of 5.75% in the one minute sit to stand test.
Top three learning points
- Team communication is vital to success.
- Do not underestimate the ability of the older generation to learn new IT skills.
- Being flexible and keeping an open mind will help drive a project forward.
Author’s reflections

‘We implemented this project in response to the pandemic in 2020 to support our isolated patients with chronic lung disease, who were not only sitting at home, often alone, but were also becoming increasingly more inactive, unfit and more breathless.
‘We continued to deliver an online virtual pulmonary rehabilitation service in Greenwich until this March. This meant we could offer greater choice for patients who would never have managed a face-to-face programme pre-Covid or during the last two years.
‘The plan now is to explore a collaboration across south east London PR services, to deliver a quality assured SEL virtual PR programme which would mean patients continue to have access to a high-quality virtual programme of care.’
More information

Number of subscribers: 1




































