A single app that helps patients self-manage any long-term condition across the whole ICS pathway may be closer than you think. Two pioneering physiotherapists are winning awards with a plan to do just that, discovers Tamsin Starr

Physiotherapists have long been at the forefront of innovating to deliver more personalised and equitable services. Now two are pioneering an award-winning way to empower musculoskeletal (MSK) patients to self-manage with a simple app that cuts waiting lists and halves prescription costs.
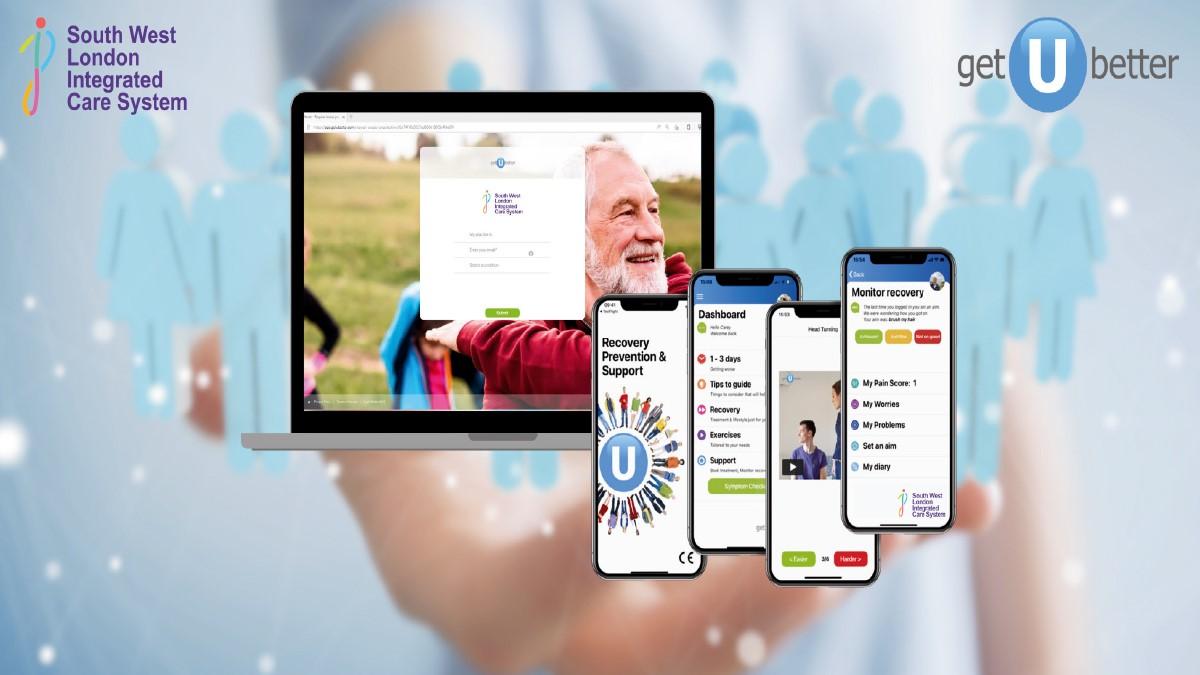
NHS South West London integrated care system spent four years co-developing an MSK self-management app (powered by getUBetter) across its entire care pathway.
The feat of joining up self-management across the whole ICS – from the point of making the first GP appointment through to community rehab – just won the prestigious HSJ HealthTech Partnership award and a shortlisting for HSJ Partnership of the Year.
Two physiotherapists were pivotal to the project – app boss Carey McClellan and Ben Wanless, consultant MSK physiotherapist at St George’s University Hospitals NHS Trust. The pair ruthlessly tested and refined the app until it was tailored to the ICS’s needs.
GetUBetter has all the usual features from a symptom checker that signposts appropriate help at all stages of a patient’s condition to self-management content like exercise videos. ‘That includes safety netting, day by day recovery, referral into the system when needed, access to rehab, support whilst waiting, patient initiated follow up, and prevention when better,’ reassures Carey.
‘But on the other side of the coin, it supports patients to have the knowledge, confidence and skills to self-manage, and use less healthcare resource.’
Patients with back pain showed an average cost saving of £1.96m per clinical commissioning group
What gave South West London’s (SWL) digital partnership the edge over other awards entrants was the team’s forensic and exhaustive testing to ensure getUBetter was fit for purpose, and Carey’s evolution of the app in response.
Ben says: ‘I’ve been the objective voice asking, “This bit doesn’t work – how are we going to improve it?” And a really good relationship with getUBetter meant there’s been an open loop of criticism, feedback and them changing and improving the app. That’s why it’s been so successful.’ Carey agrees: ‘This way, we were able to use technology to meet the needs of patients, clinicians and the health system across an integrated care system.’
Far from being a ‘digital first-NHS’ evangelist, Ben is open to digital tools only if they work in the real world. Some CSP members may even recall him arguing against the unchecked expansion of AI in healthcare at PhysioUK 2020.
And it was the real-world problems of pressured budgets and spiralling waiting lists that first prompted him to reach out to Carey.
‘Our commissioners came to us and said, “We have a problem – we’re spending too much money on our MSK back pain contract”,’ Ben explains. ‘Lots of people are seeing lots of clinicians when we know there’s evidence that people should be self-managing better.’
Ben spotted an opportunity to give patients greater control over their care at a point early enough to improve outcomes – and even help people manage themselves off a waiting list.
Reducing the ‘medicalisation’ of longer term cases and freeing up clinician time – all with necessary safety checks – promised to be additional benefits.
Effective results
Though the app’s accessibility (patients can download and use it from their GP surgery website before seeing a clinician) did ruffle some feathers when Ben began socialising the idea, the results spoke for themselves.
An independent study into the benefits of using getUBetter for patients with back pain showed an average cost saving of £1.96 million per clinical commissioning group, with a 13 per cent drop-in GP follow-up appointments, a 20 per cent fall in physiotherapy referrals and prescription costs cut in half.
Ben’s sheer tenacity in seeing the project through to completion – though he is quick to point out that there have been lots of others involved – has seen him nominated for the NHSE CAHPO digital practice award.
Chief among his clinical collaborators was Jayne Thorpe, SWL ICS’s deputy director of innovation and transformation, focused on prevention and long-term conditions.
She put her private sector background and 15 years’ experience working with start-ups into super charging the small, trust-based pilot. And as getuBetter was a new digital tech start-up, they were open to co-producing what the ICS, clinicians and patients wanted. ‘Everyone brought a different perspective and a willingness to collaborate to the table to deliver something really cool,’ says Jayne.
The programme was scaled up to support 1.7 million patients along the entire ICS care pathway. It was also extended to other chronic or long-term conditions (LTCs), including pelvic health, respiratory, heart health and pre/post-natal.
Further funding
The initial aims of reducing the 30 per cent of GP appointments that were for common MSK conditions and preventing acute patients skipping appointments were badged as ‘Covid recovery’. But early success won further funding, as Jayne explains.
‘The current SWL ICS backing to maintain the SWL digital self-management comes from the delivery of the project’s anticipated outcomes – together with continuous scrounging around for funding, and sheer determination and resilience!’
She lights up with contagious enthusiasm when discussing the collaboration’s potential to answer wider NHS transformation questions. Among them how the NHS could provide a single digital tool to support the one in three adults in SWL with LTCs to better self-manage their conditions, while also considering digital exclusion.
Patients with multiple LTCs want to be treated as people and not their individual diseases, so they don’t want different apps to manage their different conditions and commissioners don’t want to have to commission and manage multiple digital tech providers
She would like to see the app locally configured to guide people to the right care at the right time, and embedded across every patient touch point including pharmacies.
Digital innovation
Jayne’s vision may be closer than she thinks, as getUBetter is already providing its technology to more than 36 per cent of integrated care systems.
CSP heath informatics lead Euan McComiskie is optimistic that CSP members will continue to lead digital innovation across the NHS.
‘Technology and health informatics have been a core part of physiotherapy’s constant push to innovate,’ says Euan. ‘Simple and easy to use platforms like getUBetter can not only evolve in response to feedback but can collect and share good quality data to drive service improvements.’
However, he believes there are still barriers to overcome. ‘They’re still the exception rather than the norm – they’ve seen the light – that is the reason they’re winning awards.’
Though Carey and Ben cite financial pressures as the largest barriers, Euan points to successive digital competence surveys showing a mismatch between the potential of tech and our confidence in using it.
‘There are technical and competence issues, but we can work towards fixing them,’ he enthuses.
‘Sometimes the biggest challenges are finding time to address the problem identified, accepting that it will be difficult and finding the headspace to really understand it, or write a business case to fund it. But these are challenges that can be overcome, rather than barriers.’
Promoting the benefits
The team behind the CSP’s physiotherapy health informatics strategy is developing education and training to help CSP members make the most of clinical informatics.
‘Once people see the benefit they are hooked,’ adds Euan. ‘You do less paperwork, make the most of the data that you’re collecting anyway, and are able to offer this to your patients who like it more, have a better experience or achieve better, more positive health outcomes, because you’re using better tools and solutions.’
Euan believes getUBetter exemplifies the data mantra ‘collect well, use well and share well’. It’s a mantra even the resistant need to embrace. ‘In my lifetime technology will never replace a physiotherapist. But a tech-enabled physio will absolutely replace one who is not. So, there’s an opportunity for us to use tech. And when it’s used safely and effectively, it can actually address health inequities.’
He remains hopeful that the award win demonstrates the shape of things to come. ‘Those using getUBetter are changing the way that we do physiotherapy, subtly providing evidence that they’re doing it for the better.’
Find Out More
Number of subscribers: 2

