Caroline White and Katherine Jones report on the latest physio research findings.
Older patients with one or more long-term conditions may respond best to multiples strategies, with several different elements, to help them create shared health related goals and priorities with health care professionals, concludes a systematic review of the available evidence.
The researchers carried out the review because of the lack of specific guidance on shared goal setting for patients aged 65+ with several health issues. They looked at studies that compared a multifactorial approach with usual care.
They identified eight relevant studies, including five randomised controlled trials, which involved either a single intervention directed specifically at collaborative goal or health priority setting or a multifactorial intervention that included these elements.
These interventions were:
- PrefCheck, in which patients and GPs rate the importance of each health issue;
- Guided Care, comprising self-management, motivational interviewing, and caregiver support;
- Guided Care Program for Family and Friends, which focuses on enabling and supporting the carer;
- Helping Older People Experience Success (HOPE), which combines community living, social, and healthy living skills with preventive care coordinated by a nurse;
- Collaborative Care Model, which emphasises psychological wellbeing; and Integrated Systematic Care for Older People, with an emphasis on GP/nurse-led proactive integrated care.
These showed statistically significant effects on goal setting, according to the Patient Assessment of Chronic Illness Care (PACIC) goal setting subscale, as well as on the number of advance directives made, or the inclusion of goals in care plans.
These interventions shared in common an explicit focus on a clearly defined goal or priority setting by a healthcare professional and care planning.
But it isn’t clear which mix of components makes the difference, say the researchers, who add that all the studies had some methodological flaws. Neeltje PC A et al. Collaborative goal setting with elderly patients with chronic disease or multimorbidity: a systematic review. BMC Geriatrics 2017.
Need to Know
Collaborative goal-setting has been defined as ‘a process by which healthcare professionals and patients agree on a health-related goal’. [1] However, this concept is still being developed. In setting goals with patients, physiotherapists – as with other clinicians – need to find approaches for what the authors describe as ‘revealing and reconciling their own and their patients’ priorities’.
Implications?
For older adults with multiple conditions, the authors suggest that disease-specific guidelines may not always be applicable. However, the authors recognise a need for an even better understanding of what is meant by ‘collaborative goal-setting’ and ‘health priority-setting’ interventions. In turn, this could help to inform the development of relevant outcome measures for analysing and evaluating these types of interventions.
Resource
Bodenheimer T et al. Goal setting for behavior change in primary care: an exploration and status report. Patient Educ Councs 2009; 76(2):174-80.
- Katherine Jones CSP research adviser
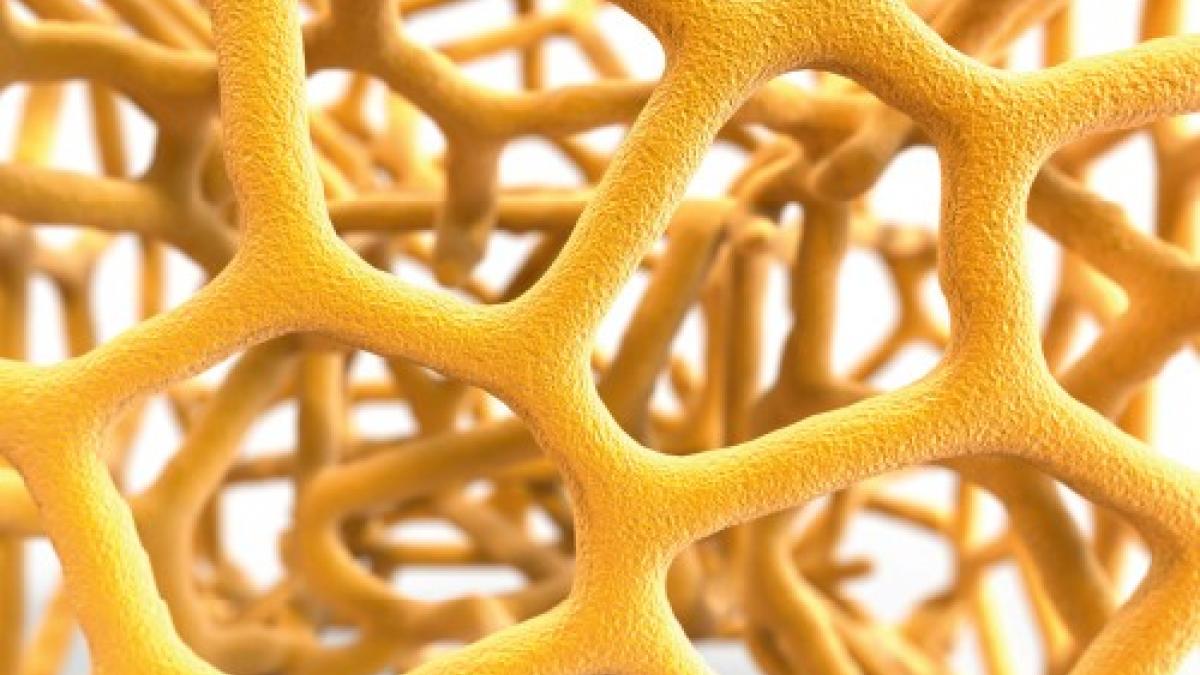
High impact exercise boosts older women’s bone density
High intensity resistance and impact training is not usually recommended for postmenopausal women with osteoporosis because of their perceived heightened fracture risk. But a new study suggests that these fears may be unfounded and that contrary to received wisdom this type of training may actually improve bone density and strength in older women.
The researchers base their findings on a clinical trial of 101 women in their mid-60s with low/very low bone density, who were either randomly assigned to 30 minutes twice weekly of supervised high intensity impact exercise for eight months or a programme of home-based low intensity exercises over the same period.
Bone mineral density of the lumbar spine and proximal femur were assessed before and after both interventions, as were measures of functional performance. These included the time taken to get up from a chair, functional reach, and back and leg strength.
High intensity resistance and impact training was more effective than low intensity exercise: it improved functional performances, bone density and strength without any side effects.
‘Even women with very low bone mass could tolerate the high loading required to increase bone mineral density as long as it was introduced gradually with close attention to technique,’ commented Dr Belinda Beck, lead study author.
‘The simultaneous improvement in functional performance suggests our exercise programme provides dual protection from osteoporotic fracture by also preventing falls,’ she added. Journal of Bone and Mineral Research 2017.
Comments & conclusions
- Night shift work increases the risk of obesity/overweight by 23 per cent, reveals a pooled analysis of 28 relevant studies. The risk of abdominal obesity was even higher at 35 per cent. Those working permanent night shifts were at greater risk than those on rotating shifts. Obesity Reviews 2017
- Older people who use steroid inhalers for asthma or chronic obstructive pulmonary disease may be more vulnerable to the risk of lung infections caused by non-tuberculous mycobacteria, finds a study of nearly 420,000 people aged 65+. While not that common, these infections are notoriously difficult to treat and resistant to several common antibiotics, warn the researchers. European Respiratory Journal 2017.
Author
Caroline White and Katherine JonesNumber of subscribers: 2




































