Physiotherapy offers safe and effective quality services that cut secondary referrals, saves money and reduces pressure on GPs.
Physiotherapy in general practice
Musculoskeletal (MSK) health issues are the most common cause of repeat GP appointments and account for around 1 in 5 of all GP appointments. Most of them can be dealt with effectively by a physiotherapist without any need to see the GP
MSK is the second largest cause of sickness absence; speeding up access to a physio will reduce this. The government changed regulations in 2022 to support patients getting advice and fit notes from their physiotherapist without having separately to see a GP.
Research shows physiotherapists are the most expert professional group regarding musculoskeletal issues with the exception of orthopaedic consultants. They have the same high safety record as GPs – and are trained to spot and act on red flags.
They are autonomous, regulated practitioners, holding their own professional liability and don’t require supervision or delegation from medical colleagues or others.
Many advanced practice physiotherapists are qualified to prescribe independently, order investigations, carry out injection therapy and plan complex case management. An advanced practice physiotherapist costs £54.11 per hour, a GP £130.71 per hour.
Modernising access
Self-referral to physiotherapy allows patients to access services directly without having to see their GP or anyone else first. Patients can either refer themselves directly into existing physiotherapy services or see a physiotherapist based in general practice.
Self-referral to physiotherapy is 25% cheaper to the NHS than a GP referral and has been fully evaluated and recommended by NICE.
Expanding the GP's team
General practice physiotherapy roles are a new form of self-referral which further develops GP and physio services, enhances patient care and reduces the GP workload.
The potential of these roles is being recognised by policy makers across the UK. In practice, change is already happening, with many GPs bringing in experienced physiotherapists to work alongside them as the first point of contact for their MSK patients. Already over 8 out of 10 GPs have confidence in this model.
GP physios usually have advanced practice skills and training. Patients with MSK symptoms can opt to see them instead of the GP to assess, diagnose, advise and provide exercises and, when needed, carry out further investigations and refer on.
What is new is that this puts physiotherapy expertise at the start of the patient’s journey, at the place they are most likely to seek help first.
Backing rehab
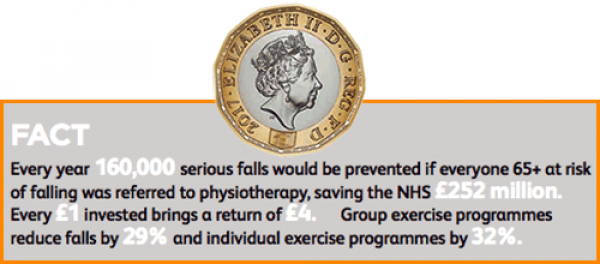
Community rehabilitation reduces the number of people becoming needlessly disabled and prevented from leading active lives. It also reduces pressures on secondary care. For example, pulmonary rehab reduces morbidity, mortality, halves the time patients spend in hospital and reduces readmissions by 26%.
Too often people receive intensive rehabilitation in hospital and just after discharge, they often have long waits when they get home, if it’s available at all. There are major variations in wait times for rehab in the community for stroke, hip fracture and COPD, in some areas patients wait up to 18-21 weeks.
In a recent study by the Stroke Association 45% of patients said they felt abandoned when they left hospital.
While patients wait their recovery is halted and can reverse – causing lasting disability, distress and deterioration of health. Half of all people who suffer a hip fracture are left with a permanent disability and can no longer live independently.
To maximise independence and reduce disability, a patient’s rehab needs to continue from hospital to home, be easy to refer back into and rooted in the community.
The UK is grappling with the same issues in primary care but in a context unique to each country.
Download the ‘Think Physio for Primary Care’ briefings for England, Northern Ireland, Scotland and Wales for evidence and examples about how physiotherapists in each country are stepping up to the challenges.
Further information
Please call the CSP Enquiries Team on 020 7306 6666 or email enquiries@csp.org.uk.
And members can get involved in the conversation by joining the first contact physiotherapy iCSP network (log in needed).



































