After decades as the Cinderella service, rehab is now increasingly talked about in the same breath as medicine and surgery. The Community Rehabilitation Alliance, which the CSP convenes and co-chairs, has used the power of more than 60 health interest groups to bring about this change, and set the scene for future transformation. In the year of its fifth anniversary, Tamsin Starr showcases its achievements and future plans
‘For decades, rehab was the Cinderella service,’ says Sara Hazzard, assistant director at the CSP and co-chair of the Community Rehab Alliance (CRA). ‘Surgery and medicine were seen as essential within the health care system, while rehab was the add on.’
CSP members will recognise the deep frustration of seeing patients not receiving needs-led personalised rehab, close to home. But establishing rehab as a right and an equal pillar of healthcare required a collective vision. A vision that could only be realised through the united power of more than 50 organisations.
The CRA – convened and co-chaired by the CSP – was formed in 2019 to do just that. Its pivotal influence grew from lobbying and getting a national accountable rehab lead in England, establishing best practice standards in all four countries and persuading senior health policy makers to use the standards to inform new and much needed national frameworks.
Similar alliances are operating with the same aims in Scotland, Wales and Northern Ireland, with increased investment seeing important wins on the right to rehab.
This year, the CRA marks its fifth anniversary, so it’s the perfect time to reflect on its journey – and its future vision.
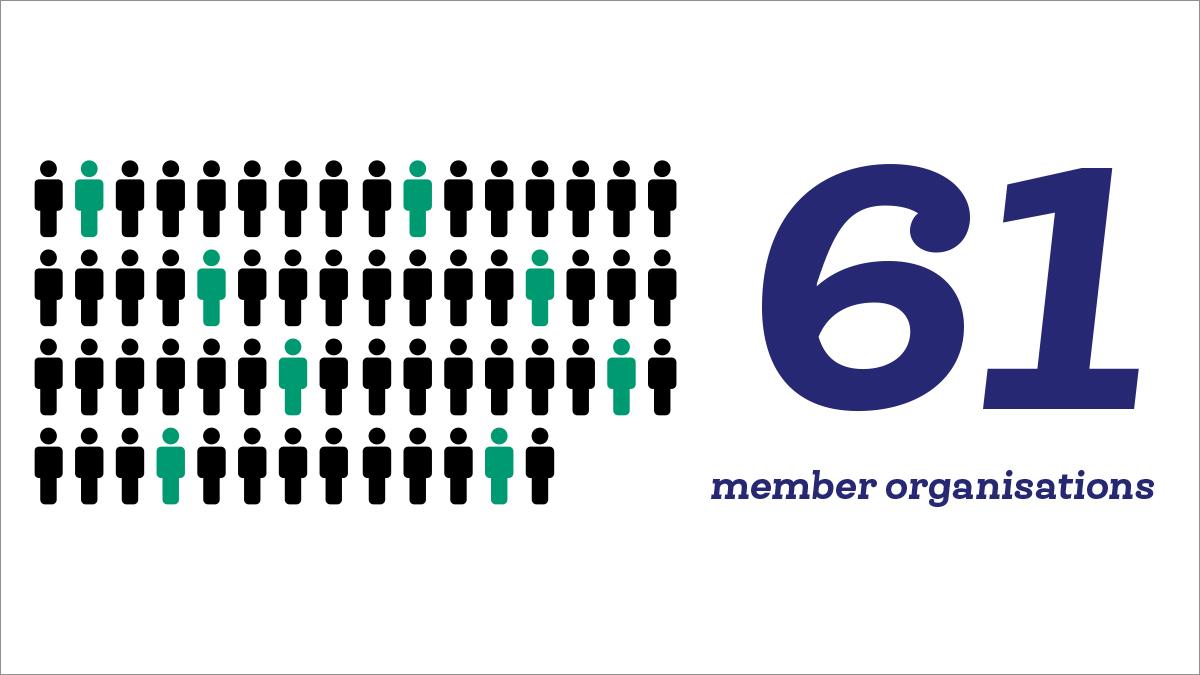
Since its launch, the CRA has gained 61 members in England. From physical to mental health, medical royal colleges to Richmond Group charities, there is unity in their commitment to rehabilitation being high on the healthcare agenda.
Personalised care
What brought members together was a shared belief in the transformative power of rehab for people and for the health and care system. Amit Arora, British Geriatrics Society vice president for workforce and one of the 2023 co-chairs of the alliance explains: ‘There was a longstanding concern that patients who had come to acute hospitals were given the rehab they wanted or needed when they were in hospital, but not outside of it. Rehab needed to continue in the community to maintain them in the physical state that they are in or to the best levels of their possible abilities. The CRA brought this out into the open, and united us around this common goal, which went outside our specialisms.’
Henry Gregg, an upcoming 2024 co-chair who represents Asthma + Lung UK on the alliance, adds: ‘Even though we’re coming at it from different specific perspectives and different conditions, we are all committed to making sure that all parts of the system are properly funded.’
At the alliance’s core is the drive for an increased emphasis on personalised care, recognising that many people have multiple long-term conditions. ’They are almost all let down when they need high-quality person-centred care close to home,’ adds Sara.
The CRA’s first joint statement set out this mission to transform rehab’s place in healthcare. ‘It was about changing the way rehab was seen from one element in an individual condition pathway to being key to treatment across multiple conditions and delivered by a multidisciplinary team that went beyond the NHS alone,’ says Sara.
Transforming rehab
Defining what good sustainable rehab would look like put them on the starting blocks to drive rehab up the agenda – both within the NHS and politically. ’In advocating for rehabilitation for everyone, we were advocating for reducing fragmentation and therefore waiting times,’ adds Amit. ‘We needed the right kind of data so we could argue for the right staff numbers, and better resources.’
Their ambition was to see accessible, personalised rehab that considered all the factors affecting people’s health, with care arranged in a sensible way and a workforce built around this approach. ‘No one gets written off as too complex, ending up back in hospital when that could have been avoided,’ Sara explains.
She continues, ‘We needed to work together to achieve this. We used the strength of being a coalition of so many health and care charities and professional bodies as a lever to lobby government and the NHS to take rehab seriously, to recognise and fund it. Now we are focusing on ensuring the workforce will be there to deliver it.’
What the alliance shows is that it that there is a strong chorus of voices – united across professions to deliver what matters most to be people’s health and care – when it comes to rehab.
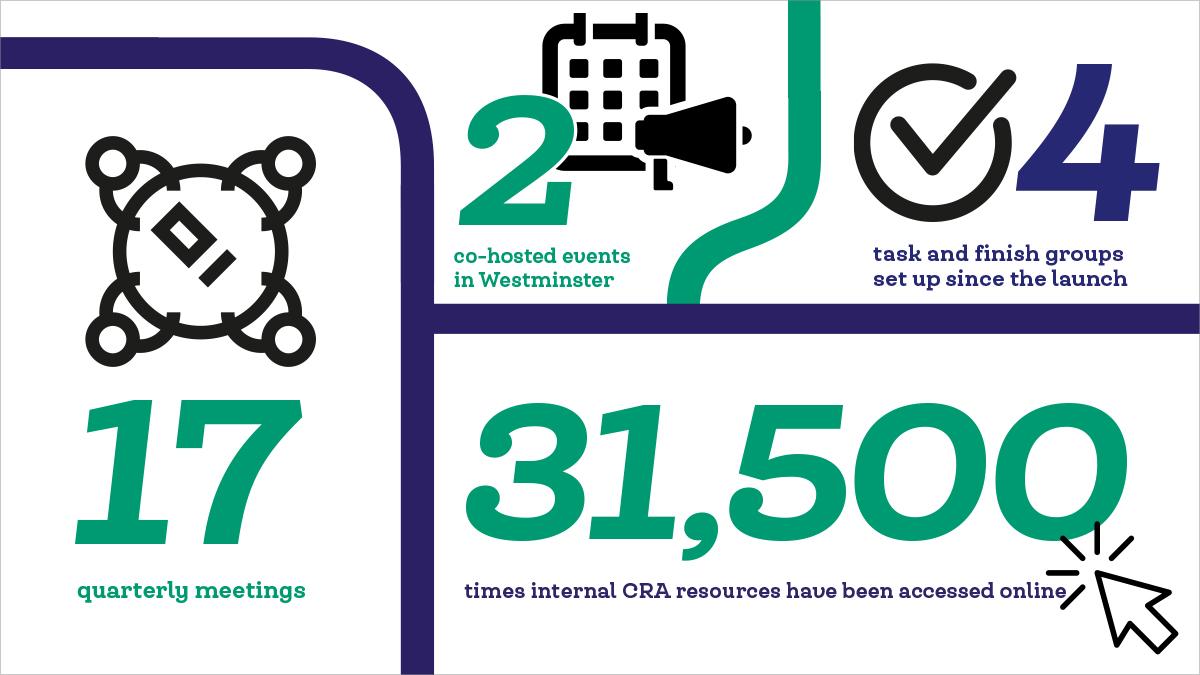
We currently have 2 working groups and 2 task and finish groups. To date, a total of 13 sub-groups of the CRA have been convened to deliver the above.
‘It can’t be about one condition or one profession pushing a narrow agenda. Our strength comes from the fact all professional groups – AHPs, nurses, doctors, exercise professionals – are standing alongside those receiving care. And we are backed by the charities covering all the big conditions, from cancer to MSK conditions,’ Sara continues.
‘This gives us more influence with decision-makers and opens doors that require a multi-profession and multi-condition approach. Anything else could be seen as out of step, self-serving or even lacking importance. The imperative is to be the solution to the wicked problems and to be the collective thinkers who know the problems are significant but not insurmountable.’
Best practice standards
A sudden acceleration to the CRA’s plans came in the unlikely form of the global Covid-19 pandemic. With the pandemic demanding new thinking for decades-old problems, the CRA was ready with the answer. The Long Covid-driven spike in rehab needs – respiratory, speech and language, psychological, loss of senses and more – left the NHS in urgent need of a new model. Spiralling waiting lists made the argument even more vital that without access to high-quality, person-centred rehab in hospital, and then in the community, patient flow breaks down. Not to mention people ending up in the most costly ends of the system – A&E or GP surgeries.
The CRA’s community rehabilitation best practice standards, published in December 2022, leveraged this to drive rehab into the planning of the newly formed integrated care boards, and health and care boards in Scotland, Wales and Northern Ireland.
Making data count
Making community rehabilitation seen and counted for had been an ambition of healthcare professionals for decades. So the CRA combined its standards with a blueprint for data collection in its Making Community Rehab Data Count report. ‘Nobody counted rehab data – and if you don’t count it, the impact can’t be measured, so you don’t fund it,’ explains Sara.
These built on an appointment the CRA pushed for in order to drive through a system-wide transformation – the role of national director intermediate care and rehabilitation, NHS England. Jenny Keane, a qualified radiographer and former Northern Ireland chief allied health professions officer, was appointed in 2021 by NHS England.
Sara explains: ‘That was the first step – that role has been intensely helpful in taking the work we did and using it to develop the standards into NHSE’s intermediate care framework and community rehab model. It also drove the urgent and emergency care plan championing the policy that people don’t just need a bed, they need rehab wrapped around it.’
Particularly welcome was the latter’s recognition of the interdependency with rehab in meeting discharge objectives intending to avoid revolving door admissions. Sara is struck by the need to not just discharge people at any cost, but to ensure people have the right care from the right people in the right place at the right time.
The framework also set out the need for each intermediate care board to appoint their own senior responsible officer for rehab. They would help transform services and align provision, optimise coordination through a local rehab provider network, as well as drive forward the all-important data gathering.
A new model for rehab
The CRA’s positioning as solution-provider took years of relentless hard work, and constant pressure, as Sara explains. ‘Relationships are the bread and butter of how you get innovation heard, seen and shared. They get you a seat at the table with decision-makers, where policy is shaped. Joint letters led to meetings and influencing that led to giving evidence, and finally NHS England adopting our model and approach.’
Still, many members remained braced to welcome – with caveats – last year’s intermediate care framework and new model for community rehabilitation. When it was published, they could not quite believe how much of their advice and input had been reflected, not to mention seeing rehab placed on a par with medicines and surgery - and the CRA credited.
‘I’m always poised to welcome the parts of new policy that are good and urge caution where it really doesn’t deliver,’ admits Sara. ‘It adopted so much of what we had created as an alliance that I had to read it twice.’
As well as the wider benefits for CSP members, being part of the alliance has also strengthened the position of the physiotherapy profession when it comes to influencing with impact.
The imperative is to be the solution to the wicked problems and to be the collective thinkers who know the problems are significant but not insurmountable
‘As the CSP, we’re always championing the role that physiotherapists and support workers play and the evidence that makes us intensely relevant as the solution. Colleagues at the CSP devote time specifically to ensure that we have influence. It does take time and commitment to convene an alliance of a large number of health and care organisations, but it has enabled us to strengthen existing relationships and forge new ones. Together we have turned up the heat when we’ve needed to, made noise when it served our common purpose and collectively normalised the language of rehab. We have had a firm focus on community services, and, when needed, on other parts of the system too, such as post-Covid return of rehab space issues.’
Workforce investment
As Sara looks forward to what the CRA can achieve in the next five years, she remains upbeat and optimistic, but under no illusion about the size of the shift. ‘It can feel an insurmountable challenge with conditions continuing to deteriorate, more needs emerging and longer and more entrenched waiting lists. But we now have the models and the standards in place to show us what we need to do differently,’ she says. ‘However, as always, the devil of implementation at scale is in the detail. We have a shared vison, which is a crucial step, but now we need a shared reality, that will only be possible with investment in a community workforce.
‘The framework and new model, which reflect the best practice standards from the CRA, show services what good rehab looks like. This is not only a sign of national commitment to rehabilitation, the like of which we’ve not seen before, it’s a trail blazed so that our members can be a part of the significant role of physiotherapy in delivering rehab.’
She is quick to add: ‘I will continue to work with colleagues and partners to campaign for a rehab workforce in the community. We need the profession to be ready for when the system creates these new positions where people need health and care. We want physios to embrace the potential for advanced practice roles in the community, support workers and rehab practitioners.’
Political influence
Asthma + Lung UK’s Henry Gregg points to positive conversations with politicians about rehab. ‘We had a very useful meeting with [former health minister] Will Quince where we talked him through what his commitment to workforce would look like in terms of rehabilitation. And how if you don’t put significant investment into that area, you’re not going to see the benefits of having more doctors and nurses, as people will keep coming back to the doctor if they don’t get better through rehabilitation services.’
A UK-wide approach
The timing – with all political parties having one eye on their general election manifestos – again seems poised to accelerate more wins. A shift to prevention has been on the table for decades, but the next general election may just open the door to longer-term thinking. ‘Progress is partly dependent on the economy and on what a future government might fund for healthcare,’ Henry adds. It’s important to make the case ahead of that money being available, so they know where to put it. And the alliance has put rehabilitation on the map and on the agenda.’
Amit continues that any wins must be reflected across the four nations. Scotland is arguably the furthest ahead, with a ‘Once for Scotland’ approach to rehabilitation published, rehab leads appointed in every Scottish health board to deliver it, and community rehabilitation best practice standards to guide implementation. It went a step further when the Right to Rehab Coalition launched a campaign and petition to have rehab recognised as a human right in Scottish legislation.
Wales has similarly published an all-Wales community rehabilitation best practice standards, with campaigning wins including a £30m investment to improve people’s chances of living at home independently. Numerous rehab policy announcements have shown that campaigning by the CSP is proving effective.
Stormont’s power-sharing collapse has slowed progress in Northern Ireland, but the CSP, working in partnership with others, has been engaging with key political stakeholders to drive the rehab and recovery agenda forward.
Amit continues: ‘We have an agreed ambition that we will develop the services for rehabilitation in the community and have equitable access to high-quality, person-centred rehab across the UK, not just in England. Across the UK we will invest and develop this alliance and its sister alliances to make that happen.’
Physios lead the way
The CRA will continue to keep the pressure on nationally to ensure that rehab is an equal pillar of healthcare and that the best way to reach people who aren’t getting rehab is to ensure access for all. Sara adds: ‘We look forward to having a similar impact on the re-design of rehabilitation services for people leaving hospital but in the future as a way of ensuring people can avoid unnecessary admissions in the first place. Rehabilitation has an increasingly important role to play in primary care, secondary care and critically in the community.
‘Our job is to ensure that at each level rehabilitation is not forgotten, and that focus is not just on people when they are in hospitals but on those in community and social care services, so that hospitals are able to help at the right time for the right reasons.’
Sara says CSP members continue to show leadership across the UK. ‘We have members leading front-runner and exemplar services as well as official pilots. We know our members are facing some of the greatest demands and stresses for at least a generation. Where and when possible, members can expect us to back their calls locally for community rehab services to be part of the workforce planning and to hold national decision-makers to account to deliver on what they have now promised.’
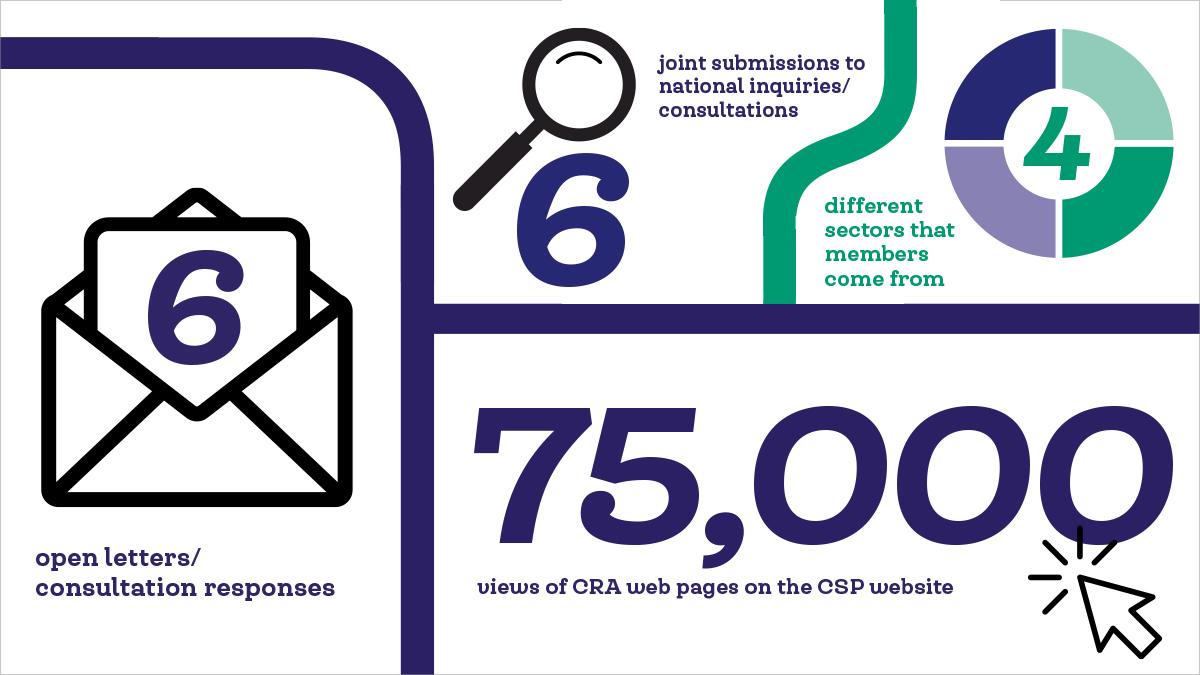
The CRA in England has published 3 reports: Rehab on Track, Making Community Rehab Data Count, and Live Well For Longer; 2 manifestos; 2 consensus statements; 1 list of asks and 1 Freedom of Information request. In addition, a virtual reality experience was created to demonstrate the impact of living without the right rehab.
Find Out More
Number of subscribers: 1




































